AUSTIN, Texas — Austin Public Health (APH) answered some coronavirus questions in a live Q&A on Wednesday, touching on a new local spike in cases.
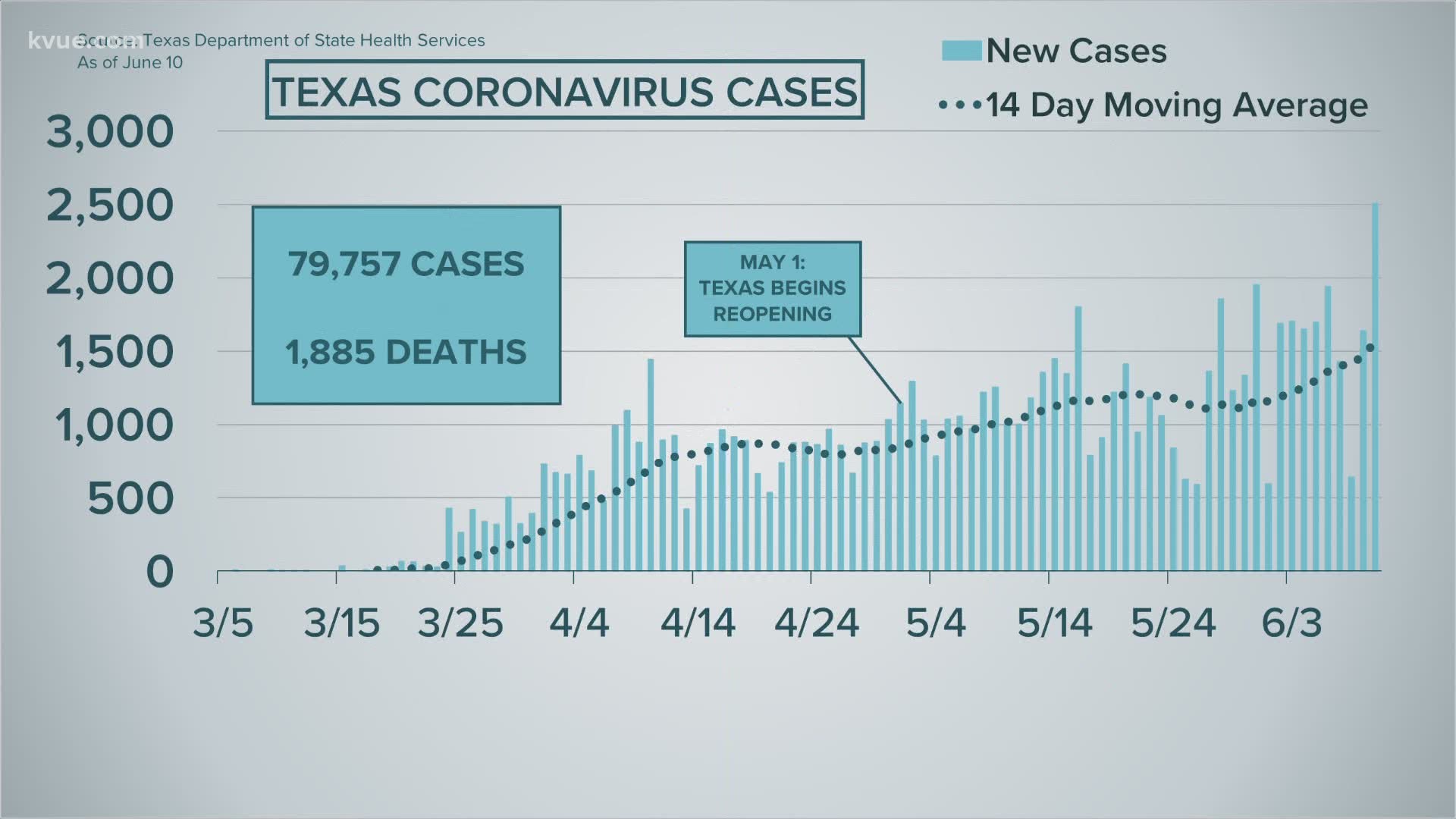
Interim Health Authority Dr. Mark Escott said there was a "concerning trend in new cases." He said on Monday, Austin/Travis County set a record for new cases at 118, and on Tuesday that record was set again at 161.
Here's a look at what local health leaders discussed:
Question: This week, Austin saw a spike in COVID numbers and Texas saw an increase in hospitalizations. Given the two-week delay, protests don't seem to be the likely cause. However, two weeks ago marks Memorial Day, so what do you attribute these spikes to?
Answer: The cases that we report over the last three days are cases that have onset of up to 10 days ago. Sometimes by the time we have a case reported, they've already recovered because their illness was onset two weeks before we got the case. So, now we are seeing an increase it seems based upon the reopening of businesses and Memorial Day activities, but also we have an increase in risk-taking behavior. What I mean by that is people are being less cautious, not wearing masks as much, and not paying as close attention to personal hygiene measures like washing your hands. We are not only going to see a week lag from when the exposure occurred to when the diagnosis occurred, but also another week lag between when the person gets sick and when they are hospitalized.
RELATED:
Question: How many people does APH have on case investigation and contact tracing?
Answer: We have about 38 staff on board that are doing case investigation. The case investigation process includes the first tier of contact tracing and following up with those initial contacts that people have identified. Over the next several weeks, we will be on-boarding additional people to assist with that effort. We have roughly 90 people identified that can support that effort. We are also accepting applications for those interested in assisting in that effort.
Question: The virus has had a disproportionate impact on the Hispanic community. What are your plans to lower the percentage of Hispanics with coronavirus in our community?
Answer: Well, we are working with other stakeholders across the community to engage in this mission. We are working on and have completed some PSAs, ensuring we have a dedicated website, which is available in Spanish on the Austin, Texas, website. We're hosting a forum this weekend to better gather information from the Latinx community.
Question: Now that all the nursing home staff and residents have been tested, what can APH tell us about problems at the facilities that have seen large numbers in cases and fatalities compared to those that have not?
Answer: We're still analyzing some of the data, particularly since the widespread testing has just come back. The evidence does seem clear that once an outbreak has taken hold of a facility, it is very hard to stop. That means we have to be aggressive when it comes to screening. Particularly when it comes to staff screening. I reported last week that, so far, our positivity rate for residents of nursing homes who had no known cases was 0.17%. For staff at those same facilities, it was 0.05%. So, the rates of positivity are very low across those facilities that have no known outbreaks.
RELATED:
Question: The virus continues to affect Austin's communities of color disproportionately. What can public health officials do in the future to reduce this inequity after the virus is gone? What are some lessons learned to help those communities going forward?
Answer: This goes back to the fact that we must address the social deterrence of health that are leading to the disproportionate impact in terms of hospitalizations and death in communities of color. This shouldn't be a surprise to anybody that this is affecting those communities more than others. We know that diabetes is the same way. We know that cardiovascular is the same in terms of disproportionate risk. We've got to work harder as a community to address these inequities. It's inexcusable as a country that in 2020 we don't have access to care for all members of our community. Primary care is relatively inexpensive to provide to people and should be the first target of any federal or state legislative action. Let's just provide people primary care so they can be screened for diabetes, for hypertension, for cardiovascular disease.
Question: Why did you shut down a testing site yesterday due to heat? As we get further into the summer, how do you plan to keep testing sites running with people in heavy PPE gear in high temperatures?
Answer: First of all, we certainly apologize to those who had to reschedule their testing due to a couple of issues. All the individuals that were turned away have been rescheduled. The first issue is we had a technical issue with scheduling, which over-scheduled individuals for testing at the site. We had our personnel, some of which are City of Austin personnel, and others from hospital systems, who were certainly willing to stay as long as they needed to test the rest of the folks. But, due to the heat and conditions while wearing PPE, there was substantial concern for potential of heat exhaustion or heat stroke if they continued for additional hours to test. Going forward, we are addressing the staffing and hours of operation, as well as the rotation of staff.
PEOPLE ARE ALSO READING: