FALFURRIAS, Texas — This story originally appeared in The Texas Tribune.
After 8 a.m. on a fall Friday, a 31-foot white van drove down pockmarked streets, passed a public housing complex and pulled into the Falfurrias High School parking lot. Masked medical staff unloaded coolers filled with vaccines, then unpacked gloves and bandages. Others set out a hot pink sign bearing a handwritten message: “Free Flu Shots!”
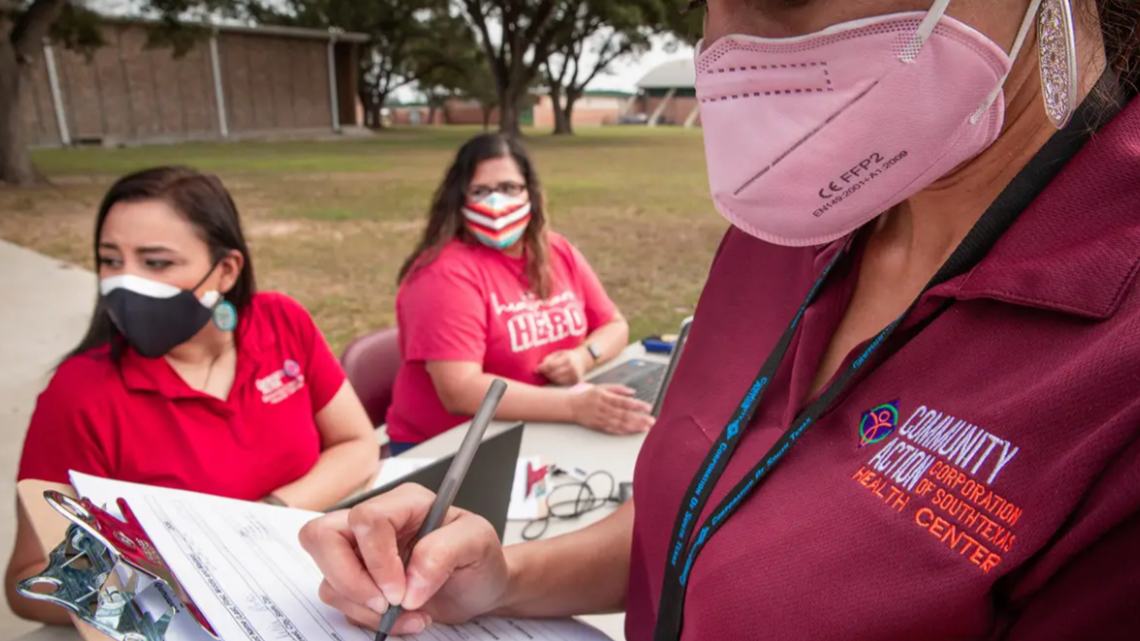
The nonprofit Community Action Corporation of South Texas has given flu shots for years in Falfurrias, a city of some 5,000 with one major grocery store and a health clinic with a worn facade. The mobile unit, introduced this year, is meant to reach people who might not get vaccinated — those who live in remote areas, depend on family members or neighbors for transportation or don’t regularly see a doctor.
“We don’t have too many providers … our closest hospital is 45 minutes away,” said Maria Rodriguez-Casas, the school district’s superintendent. “So this accessibility is great.”
Now a vaccine for the coronavirus is on the horizon, and Gov. Greg Abbott has said the state is ready to swiftly distribute doses to combat the pandemic, which has already claimed more than 20,000 lives in Texas and dealt the economy a severe blow. But health officials say tried and true distribution methods in Texas may be insufficient for coronavirus vaccines that require subzero transportation and storage temperatures and require people to come back for a second dose.
The stakes are enormous. How effectively public health officials can prioritize and distribute millions of doses of the new vaccines across a state that covers 270,000 square miles and more than 170 rural counties will determine how quickly Texas turns a corner in a pandemic that is again surging across the state and pushing hospitals to the brink in West Texas and the Panhandle.
The task is made more difficult because the Texas Department of State Health Services, which is largely responsible for the distribution effort, won’t know which vaccines it’s receiving, and how many doses, until one or more is approved by the U.S. Food and Drug Administration.
They will also have to combat misinformation and persuade vaccine skeptics — and those unnerved by the coronavirus vaccines’ historically swift development — of the benefits of being inoculated. World Health Organization experts have said that up to a 70% vaccine coverage rate for COVID-19 may be needed to reach population immunity through vaccination. In the 2019-20 flu season, only about 37% of adults younger than 65 received a flu vaccine. The rate was about 65% for seniors.
“We haven't seen any efforts that are this broad since probably a polio vaccination in the 1950s,” said Dr. Mark McClellan, a former head of the FDA who has advised Abbott about the pandemic.
“The people who are most likely to benefit from vaccination are people who may have difficulty connecting to health care,” such as elderly people and residents of low-income communities who often lack health insurance, he added — compounding the logistical challenges.
The vaccine is expected to initially be in short supply, and will be first distributed to a state-selected group of people considered to be essential workers or most vulnerable to being severely sickened.
In most other respects, the distribution process is being dictated and paid for by the federal government, which has said the vaccine will be free to vulnerable people who can’t afford it and that providers will be able to bill health insurers for immunizing covered patients. The Trump administration has partnered with pharmacies like CVS and Walgreens to offer the vaccine to nursing home residents and workers and, later, the general public, once supplies become more available.
Health officials in Texas, meanwhile, have sent the federal government a rough plan for how they will prioritize getting vaccines to populations that need it most. They are now quickly recruiting pharmacists and doctors to sign up to receive shipments of a vaccine, and trying to teach providers how to use an electronic system to record vaccinations and track when people are due for a second shot.


Of Texas’ 254 counties, 38 didn’t yet have a provider signed up to receive vaccine shipments as of Nov. 18.
The vaccine planning is happening as coronavirus infections are soaring in the state, a fatigued public grows reluctant to follow rigid safety guidelines and state officials say they are uninterested in renewing more aggressive steps to tamp down the virus’ spread, such as ordering nonessential businesses to close.
The situation has grown so dire in El Paso that inmates are being paid $2 an hour to move bodies into temporary morgues. Medical tents have popped up outside packed hospitals from El Paso to Lubbock.
With two pharmaceutical companies announcing that they are close to requesting FDA approval for the vaccines, it’s looking increasingly likely that immunizations will begin while the pandemic is still raging.
“The last thing we want to do is have people lining up to get a vaccine and then catching COVID while they're waiting for the vaccine to kick in,” said Dr. Philip Keiser, a physician at the University of Texas Medical Branch and a co-chair of its vaccine distribution task force.
“We're in a very funny spot because we're trying to figure out how do we be efficient and how can we be extremely careful … while still working with a wide degree of uncertainty about what it's going to look like,” said Keiser, who is also the Galveston County health authority.
Preparing for a vaccine
Pfizer and its German partner BioNTech, and Moderna, makers of the two vaccine candidates that are furthest along in development, have predicted that they could be able to produce enough vaccine doses for some 20 to 30 million Americans — a fraction of the U.S. population — before the end of the year.
Unlike a run-of-the-mill flu shot for adults, both companies’ coronavirus vaccines require people to get a second shot to be effective, and the Pfizer vaccine must be stored at ultra-cold temperatures — requiring specialized freezers that so far only about 120 providers in the state say they have access to.
Moderna’s recent announcement that its vaccine can be stored for 30 days in a standard refrigerator is a “game changer” for the state, said Imelda Garcia, associate commissioner for the Texas Department of State Health Services’ Division for Laboratory and Infectious Disease Services. That expands the number of providers who can store the vaccines to more than 2,000, she said.
Under health experts’ most optimistic predictions, most people are still months away from having easy access to coronavirus vaccinations. But those experts worry that “euphoria” over Pfizer and Moderna’s recent announcements could make people feel less urgency to take precautions like wearing masks and social distancing.
“If somebody dies between now and February when the vaccines become available, it’s especially tragic because every single death from now on is preventable,” said Dr. Peter Hotez, dean of the National School of Tropical Medicine at Baylor College of Medicine. “It’s like somebody dying in the last days of the Civil War or World War I.”
It’s still unclear, beyond a list of murky priority groups such as health care workers, who will get the vaccine during the initial months when supplies are scarce. In the coming weeks, a state panel of experts is expected to publish more specific recommendations about who will be eligible for a vaccine and when.
Early estimates from the Texas Department of State Health Services found there are more than 5 million people who are vulnerable or work in front-line jobs that increase their exposure risk. That includes more than 3.9 million people who are 65 or older, more than 638,000 health care personnel, more than 327,000 acute care hospital employees, more than 137,000 nursing home residents and more than 66,000 emergency medical workers.


The state’s adult population also includes more than 9.4 million Texans with underlying medical conditions that could increase their risk for severe illness associated with COVID-19.
Garcia, with the Department of State Health Services, said the state has hired more staff to prepare for vaccine distribution and enroll providers. Information technology staff are making sure the expected volume doesn’t overwhelm the state’s electronic immunization tracking system, an essential tool needed to report anonymized data to the federal government.
National associations for state health officials and immunization managers have asked Congress for at least $8.4 billion to pay for efforts to distribute the coronavirus vaccine, and Centers for Disease Control and Prevention Director Robert Redfield has said that some $6 billion would be needed.
Texas has received roughly $14 million from the federal government so far, with $10 million earmarked to send teams out to distribute the vaccine, Garcia said. The federal money may not be enough to cover local governments’ costs for setting up and staffing vaccine clinics.
“That is a concern,” she said.

Concerns about distribution
Dr. David Lakey, chief medical officer at The University of Texas System and a member of the state’s expert panel for vaccine allocation, said the challenge of prioritizing who will get the first doses of a COVID-19 vaccine reminds him of the state’s 2009 distribution of the H1N1 flu vaccine, which he oversaw.
“When you start adding in anyone that has a chronic disease into a priority group, all of a sudden that number gets very big,” he said.
During that round of flu vaccine distribution, the U.S. government “would overpromise and then underdeliver with the supply,” Lakey said, which meant state and local officials had to abruptly change plans about which priority groups were eligible to receive a vaccine in a given week.
Early data suggests the COVID-19 vaccines in development are safe and effective, Lakey said, but because they rely on new biotechnology, public health officials need to work especially hard to build trust in high-risk communities. That could mean working with physicians of color, religious leaders and community organizers to help promote vaccination efforts.
“Historically, there have been incidents where people of color were not treated well by the medical establishment, and there will be a concern in communities of color of how well will they trust this vaccine,” Lakey said.
Health experts are equally concerned about vaccinating people in Texas’ most rural pockets, where medical professionals are scarce and struggling small-town hospitals have been closing.
State officials have discussed sending specialized teams to people in rural areas or long-term care facilities who may have difficulty getting to pharmacies, doctors’ offices or public health sites. The Department of State Health Services says it may arrange such teams, as could local health departments or the state’s division of emergency management.
Dr. John Gibson, UNTHSC assistant dean of rural medical education at the Texas College of Osteopathic Medicine, said pharmacy chains won’t be able to go out into a rural community and deliver vaccines, and residents can’t be expected to drive to an urban center.
“I’m exceedingly concerned about this,” he said of the vaccine’s distribution. “Rural areas often don't even have a full-time pharmacy” and personnel may be “up to their eyeballs in just taking care of sick people.”
His worry is so great that he is trying to arrange for doses of the vaccine to be sent to the Health Science Center, in Fort Worth, which has cold storage units, so that he and his medical students can go out in a van to immunize at-risk or vulnerable residents in the surrounding areas.
In rural areas, worries about supply and money
He and other public health professionals are most concerned about reaching people like Christina Garza, 36, who visited the Falfurrias flu clinic in November. A cashier at a Stripes convenience store, she learned about the clinic when a flier was dropped at her work. She doesn't have health insurance, she said, and doesn’t normally get a flu shot.
She wouldn’t have gone to a doctor’s office for a shot, she said — “my kids, yes, but not me because I don’t have insurance.”
The Community Action Corporation of South Texas runs seven health centers and offers social services across 18,000 square miles. For flu clinics, it parks a mobile unit at a well-known and easily accessible landmark like a school, said Ann Awalt, executive director of the nonprofit.


But she has major concerns that her organization won’t receive enough doses of the coronavirus vaccine— or have the cold storage capability — to send mobiles out to the small towns it serves, or bring people in. The health center struggled to get enough supplies like swabs, through private sellers, to set up drive-through coronavirus testing earlier in the pandemic, and she is worried the same could happen with the vaccine, she said. Because the coronavirus tests had to be frozen, they would race an ice chest back and forth between mobile COVID-19 test sites and their office.
Another unknown for the nonprofit, which treats a large number of uninsured people, is how they will pay for such a huge undertaking when a vaccine arrives.
Whether the nonprofit takes the vaccine into communities or people come to the health centers for their shots, there will be a cost that must be covered, Awalt said.
“We’re really hoping that there are federal funds similar to the CARES Act,” she said, referring to an economic relief package passed by Congress in March. Likening rural and economically needy parts of big cities to health deserts, she said “we have some ideas about how to get people to the vaccine but it… requires some financial assistance.”
"It will be confusing at first"
While the state’s flu vaccine distribution model is well-established, some clinics say there have been disruptions this year that leave them worried about the logistics of a COVID-19 vaccine.
“If you look at the distribution of the flu vaccine as the dress rehearsal for COVID, we’re in trouble because it hasn’t gone very smoothly,” said Jana Eubank, executive director of the Texas Association of Community Health Centers.
She said many of her association’s member clinics this year haven’t received flu vaccine doses they expected from the state and have been left to try to buy them on the private market instead, reminiscent of difficulties they faced earlier this year in acquiring personal protective equipment as the coronavirus pandemic reached the U.S.
And for many of the low-income patients they serve, making a trip to a clinic to get a shot involves other hurdles: finding transportation, child care or time off work. In some rural areas, it may require a drive of an hour or longer.
“Let’s say we get them to come in for that first vaccine and then they feel really badly, run a fever, achey, miss a couple of days of work,” Eubank said. “They might say, ‘Wow, this isn’t worth it. I’m not coming back for [the second dose].’”
A spokesperson for the state health services department said the agency was not aware of widespread issues with flu vaccinations.
Austin Public Health officials set up a flu clinic on Nov. 7 at a county exposition center, not just to help people get an influenza shot, but to test their capacity for performing large-scale clinics for an eventual COVID-19 vaccine.
The agency dispatched staff nurses as well as nursing students and pediatricians in training. They took pre-scheduled appointments as well as walk-ins. Over five hours, the clinic immunized 426 people.
Cassie DeLeon, an interim assistant director at the health department, said it was too early to know what models it will use for COVID-19 vaccination, but she said options include similar walk-in clinics, converting COVID-19 mobile testing sites into vaccination sites and drive-through clinics.
“I think the main thing for everyone to understand is just because we have a vaccine, we still have a pandemic that we have to manage, so we will be in this a long time,” she said. “That’s the grace that we’re asking. I know we have pandemic fatigue happening … [but] continue to practice those safety protocols of social distancing, wearing your mask, handwashing.”
Keiser, the Galveston health authority and physician at UT-Medical Branch, said they’re unlikely to send mobile clinics out initially, in part because the leading vaccines require two doses that must be given three to four weeks apart.
“It’s not something where you just set up in a parking lot and say, ‘Y'all come,’” he said.
“I can promise you one thing, it will be confusing when it first starts,” he said. “I can promise everyone that we're going to do the best we can to make sure that we can get [to] everybody as quickly as we can.”
Disclosure: Texas Association of Community Health Centers and University of Texas System have been financial supporters of The Texas Tribune, a nonprofit, nonpartisan news organization that is funded in part by donations from members, foundations and corporate sponsors. Financial supporters play no role in the Tribune's journalism. Find a complete list of them here.
The Texas Tribune is a nonpartisan, nonprofit media organization that informs Texans — and engages with them – about public policy, politics, government and statewide issues.

