'I felt cheated. I felt robbed.' | Central Texas mothers share their experiences with postpartum mood disorders
KVUE spoke with more than 100 women about postpartum mood disorders in order to get a better understanding of what women can experience after giving birth.

They may not be "normal," but they're a lot more common than most people think.
Postpartum mood disorders – like depression, anxiety, OCD and PTSD – affect so many mothers, yet many women choose to suffer silently.
But not anymore.
KVUE spoke with more than 100 women in the Austin-Round Rock area about postpartum mood disorders in order to get a better understanding of what women can experience after giving birth.
Our hope is that by sharing their stories, other mothers can feel like they are not alone and that there is hope.
Understanding the Difference Postpartum depression isn't the only postpartum mood disorder mothers can experience
There are several different ways postpartum mood disorders – sometimes referred to collectively as postpartum activity or postpartum distress – can present themselves. Sometimes they start before or immediately after giving birth and other times it can take weeks, even months or up to one year after delivery for the symptoms to fully present themselves.
People might be familiar with postpartum depression, but it's not the only postpartum mood disorder. Here's a breakdown of some of the most common disorders:
Postpartum depression (PPD) is one of the most common diagnoses. Approximately 15% of new mothers will experience PPD. According to the National Institute of Mental Health, symptoms of PPD include feelings of sadness and anxiety that might interfere with a woman’s ability to care for herself or her family. She may also cry more often or for no apparent reason, have trouble sleeping or sleep too much and have thoughts of harming herself or her baby.
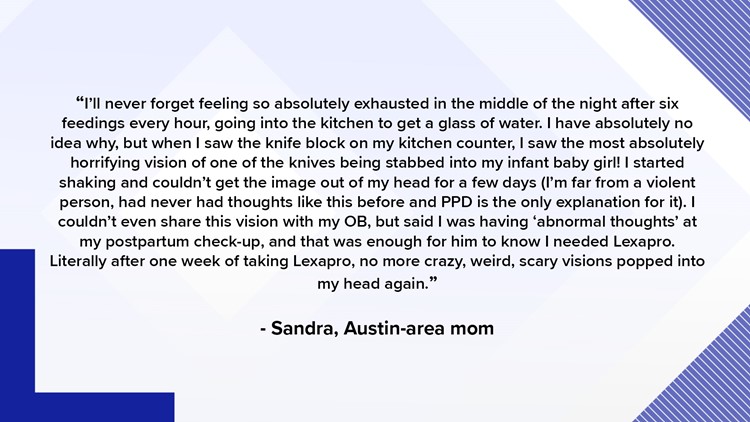
"I’ll never forget feeling so absolutely exhausted in the middle of the night after six feedings every hour, [and] going into the kitchen to get a glass of water. I have absolutely no idea why, but when I saw the knife block on my kitchen counter, I saw the most absolutely horrifying vision of one of the knives being stabbed into my infant baby girl!!!! I started shaking and couldn’t get the image out of my head for a few days (I’m far from a violent person, had never had thoughts like this before and PPD is the only explanation for it). "I couldn’t even share this vision with my OB, but said I was having ‘abnormal thoughts’ at my postpartum checkup, and that was enough for him to know I needed Lexapro. Literally after one week of taking Lexapro, no more crazy, weird, scary visions popped into my head again...Thanks for letting me share this with you privately as this is never been shared before, and I shared it to help you add to your data collection that PPD is a very real and scary thing!" – Sandra, Austin-area mother
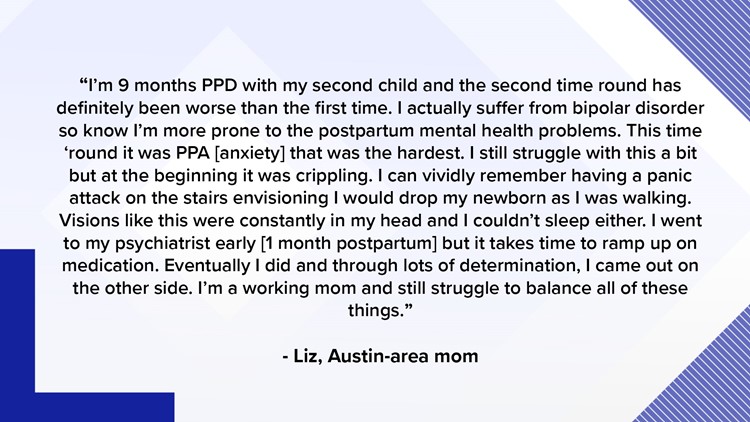
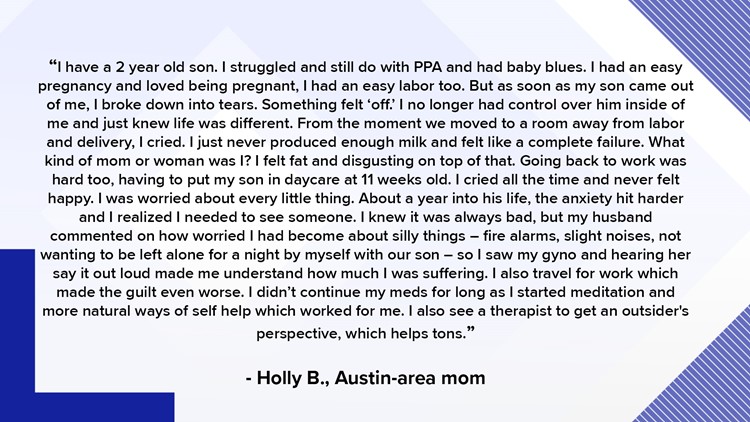
Postpartum anxiety (PPA) has similar symptoms and affects up to 10% of new mothers. Many mothers with PPA have racing thoughts that they have difficulty controlling – like that something bad will happen to their child – and they cannot concentrate, sleep or eat properly because of those thoughts, according to AmericanPregnancy.org.
"I began imagining morbid scenarios in which I was the accidental cause of my baby’s death or injury. I wouldn’t take her near stairs because I was afraid I’d drop her. I wouldn’t take her near a balcony because I was afraid I’d drop her. I wouldn’t do anything if it even remotely caused me to fear an implausible scenario of me accidentally harming her. I had intrusive thoughts of her dying. I was sick. Mentally and physically, I felt sick. I had never experienced this before, and I began to feel guilty for feeling sick." – Hillary, Austin-area mother.
Postpartum OCD, while less common, affects 3% to 5% of postpartum women. Symptoms can include being afraid of being alone with the baby and being overly occupied with keeping your baby safe. Women may also do things over and over to try and calm their fears, like listing or counting things and repeatedly cleaning or feeding the baby beyond the "normal" amount of times.
"An undiagnosed lip tie made it impossible to breastfeed my first son. I bled for every feeding and it left both of us in tears, to say the least. I was determined to give him breast milk so I exclusively pumped for 8 months, but the damage was done. I felt like a failure. I told my husband I felt inadequate to be a mother and found myself crying often. Then the anxiety and OCD kicked in. I’d imagine myself falling down the stairs with the baby or waking up to his face pressed downward in his bassinet. The bottles and nipples had to be perfectly aligned or I’d find myself in a panic. It wasn’t until I stopped 'breastfeeding' that I started to feel better. But I still haven’t forgiven myself." – Celina, Austin-area mother.
Postpartum PTSD primarily affects women who have a traumatic birth or a birth that they think was traumatic and varied from their idea of what it would be like. Situations like an unplanned C-section, emergency complication or a baby rushed to the NICU can trigger post-traumatic stress symptoms in new moms. Women may have flashbacks of the birth or feelings of re-experiencing the panic of the birth as well as anxiety and panic attacks.
"I went into labor around 10 p.m. on a Tuesday, and he was born at 9:30 the next morning. He got stuck on his way out, and it was almost an emergency C-section. He inhaled amniotic fluid into his lungs for his first breath at life, and that's where his trouble started. But in the months after he was born, I started having thoughts about all the different ways he could die, then I would get angry at nothing at all. Emotions I couldn't control." – Stephani, Austin-area mother.
Postpartum psychosis is much rarer. The onset is quicker, more intense and involves a loss of grounding with reality. It may involve hearing things others don't hear, delusional thinking or intrusive thoughts.
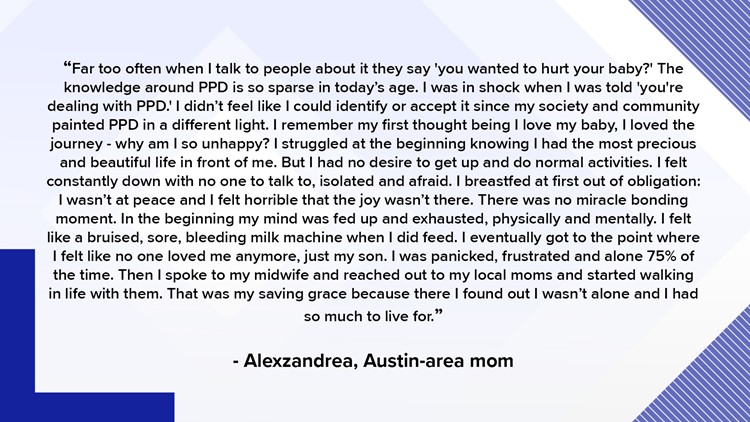
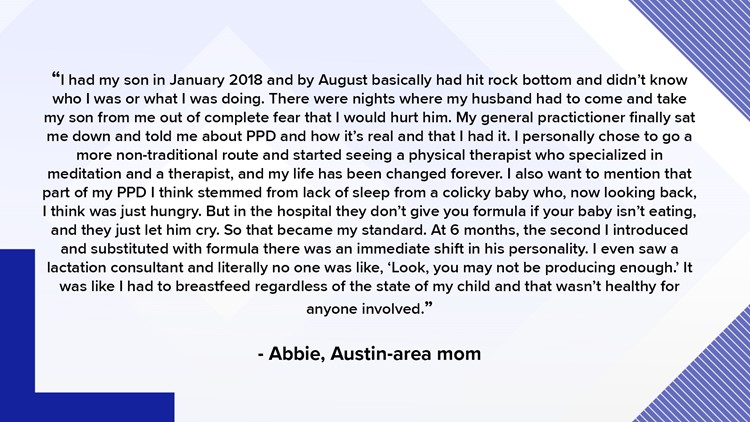
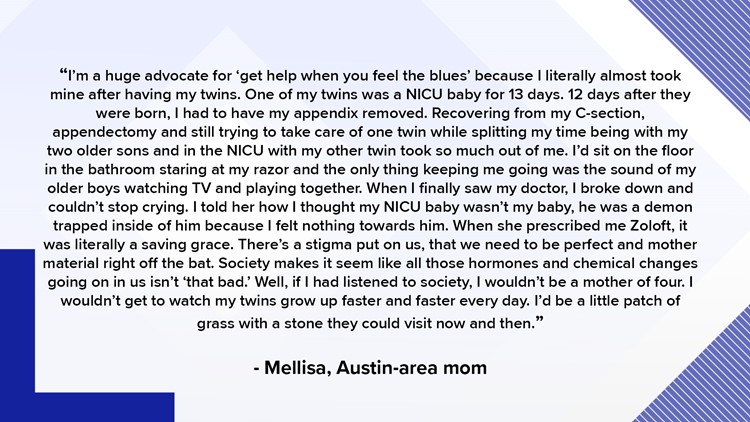
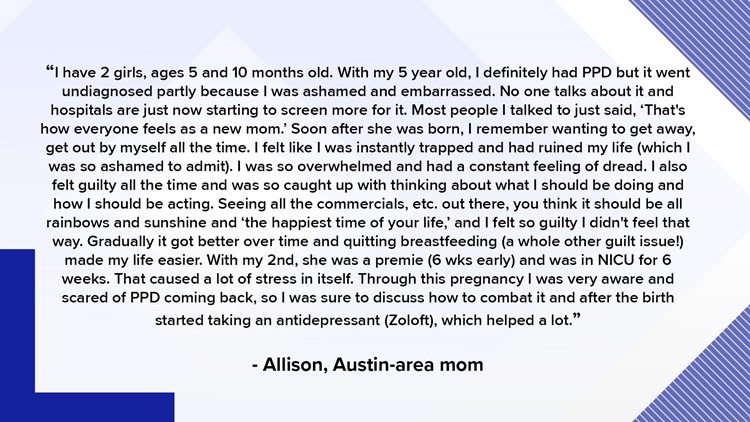
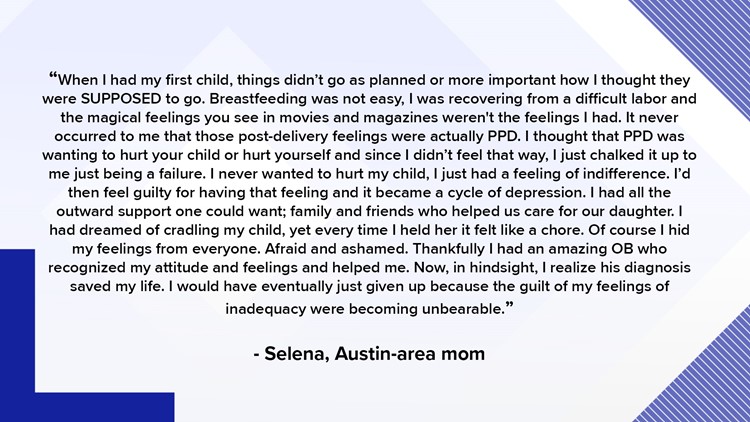
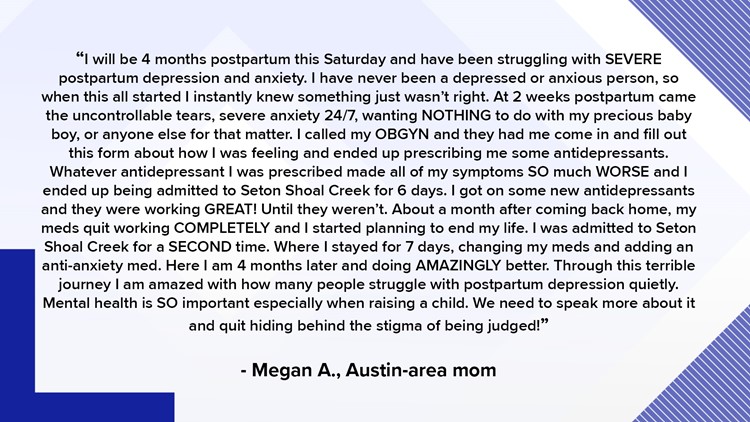
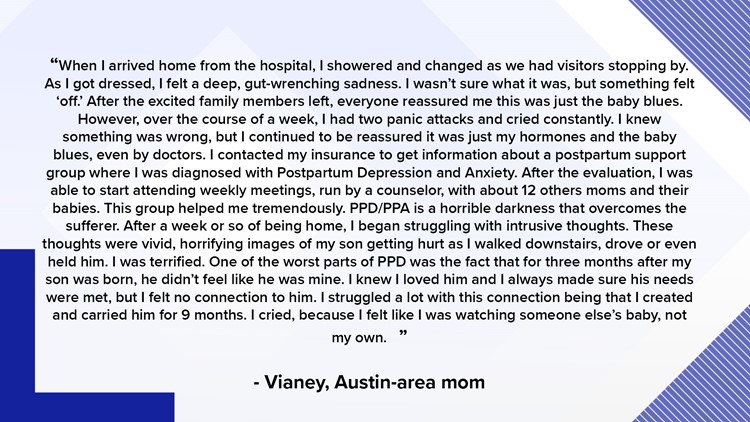
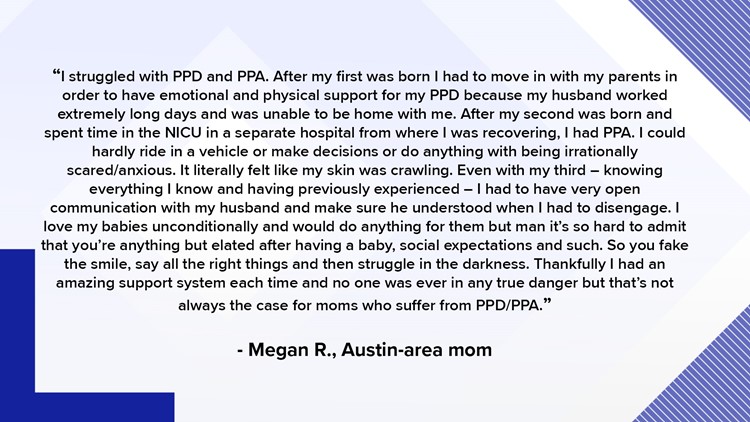
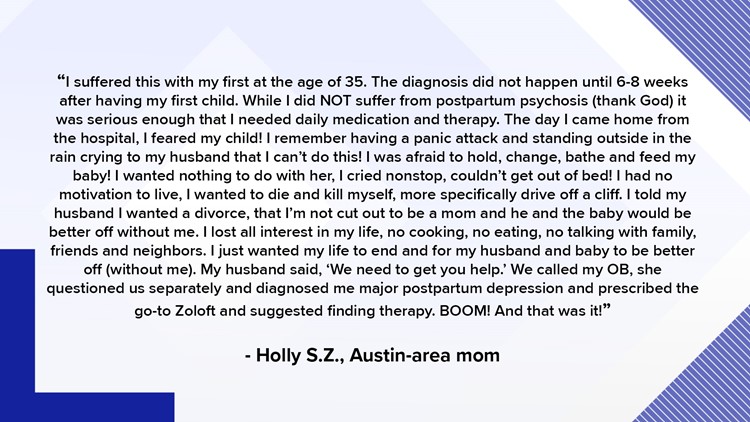
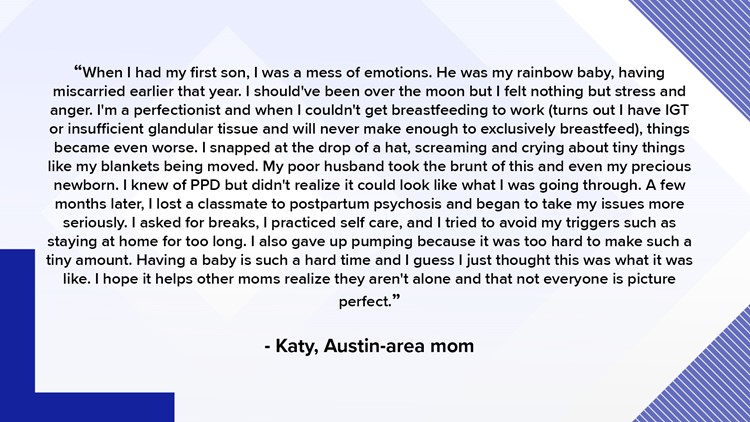
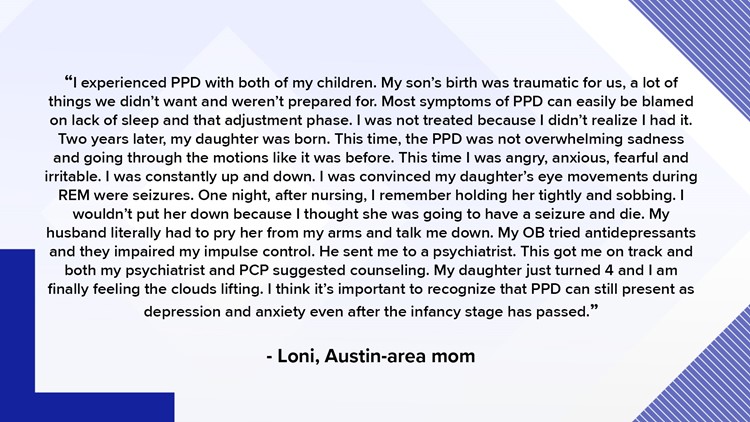
GALLERY: Austin-area moms share their experiences with postpartum distress
Jessica's Story Jessica had postpartum depression after delivering her third child
It wasn't her first time giving birth, but when Jessica DeVoss delivered her third child, Winnie, she knew immediately something was wrong.
"Everything was normal but I felt that I wasn't. I felt a disconnect between me and her because I had had these two other children, which I think is helpful, because I knew what it felt like to be immediately bonded," Jessica said. "I didn't feel that with Winnie...I didn't feel love for her."
While she was in the hospital, Jessica realized she was suffering from postpartum depression.
"I knew something was off. I didn't say anything because I thought, first of all, 'Maybe I'm just tired,'" Jessica said. "I knew I had postpartum, I knew it and it was depressing, it was very sad because I wanted to love her. I tried."
Instead, all Jessica felt was obligation toward Winnie. She breastfed her daughter to try and keep that connection, but it was more out of obligation.
"All I felt for this beautiful baby was obligation. That was the beginning and ending of my feelings," Jessica said.
Then, several months after Winnie was born, Jessica said she hit her lowest point.
"I very much came to the end of myself somedays, but this particular time I was sitting trying to nurse her and she just wouldn't nurse and she was fussing and I had this thought that I could put her in her car seat and take her to the hospital and drop her off and that would be better for her. And then I thought that she would die if I didn't love her because she could feel that I didn't love her," Jessica said. "She was maybe three months old."
That's the night she told her husband what was going on and realized she needed to do something to change how she felt. She initially tried antidepressants, but they didn't have any effect on her. They also appeared to dry up her milk supply, and she didn't want to give up breastfeeding since it was the only way she felt connected to her daughter.
Eventually, Jessica joined a support group at church and began to feel more like her old self. It was faith and time, she said, that eventually saved her.
"It was about a year before I could look back and say, 'Wow, that was really hard, I'm so glad that's over,'" Jessica said.
Still, she felt like the first year of her daughter's life was stolen from her.
"I felt cheated. I felt robbed."
Kelly's Story Kelly had postpartum PTSD and depression after a complicated pregnancy and birth
At 20 weeks pregnant, doctors advised Kelly Patterson to terminate her pregnancy.
Her daughter was diagnosed with a congenital diaphragmatic hernia (CDH), a defect in the diaphragm that is often fatal for newborns.
"She had slim to no chance of survival and even if she did make it, they told us that she would only live for maybe a few days," Kelly said.
But for Kelly and her husband, abortion wasn't even an option.
"We had already lost two babies via miscarriage, and we were desperate to be able to have our second child and we were not going to give up. We were at least going to be able to meet her, even if long-term we weren't going to be able to keep her," Kelly said through tears.
They found a CDH specialist and at birth, Kelly's daughter, Charlotte or "Charly" as they like to call her, was immediately placed on life support.
Kelly didn't even get a chance to hold her.
"She didn't cry, she barely made any noise. She was pretty purple, blue because she couldn't breathe," Kelly said. "[The doctors] stopped for a second, I grabbed her hand and that was it."
Charly was rushed to the NICU and remained in the hospital for several months before she was strong enough to come home.
The first year of Charly's life was spent focused on her survival and care, Kelly said.
It wasn't until Charly turned one that Kelly realized she, as a mother, was now suffering from postpartum depression and PTSD.
"I completely isolated myself from everybody, and it took me a very long time to realize what I was doing," Kelly said. "It's hard to admit that you can feel so depressed after having a child that you're lucky is there to begin with."
Then, this past December, Kelly said she hit her lowest point when she began having suicidal ideation.
"I honestly thought it was the best solution. And I left the house one day, it was the middle of the day and I just...it was too much. And I drove to the park and I called my best friend, thank God, and I finally said it out loud to somebody for the first time," Kelly said. "That was kind-of the turning point for me, where I could see long enough and clear enough that I needed to get to a doctor and I needed to see a therapist and I needed to start investing in myself so I could be there for her."
Now, thanks to medication and therapy, Kelly said she is slowly recovering from symptoms of PPD and postpartum PTSD.
"I have good days and bad days," Kelly said as she played with Charly, now two.
Both Kelly and Jessica wanted to share their story in hopes that they help other women who may be struggling.
Q&A with a Professional Christine Hall is a psychologist who specializes in postpartum counseling
We sat down with Dr. Christine Hall, an Austin psychologist that specializes in postpartum counseling to ask some questions about treatment.
Kris Betts: What do you tell women who feel guilt and shame for experiencing a postpartum mood disorder?
Christine Hall: The guilt and the shame are huge, and the stigma is huge because when you have a baby, everybody around you is excited that you're pregnant, there's a lot of joy and happiness. And so you get the message that something is wrong with you if you're experiencing some of these symptoms. Then you start to internalize that because you're not as happy as everybody thinks you should be, and family members may tell you, 'Oh, just get more sleep.' But with these symptoms, oftentimes sleep and rest do not come easily. So helping new moms understand yes, there is a stigma attached and yes, women do experience this and it's okay, we're going to get you through this. Also explaining that you've lost the hormones that were necessary to carry the pregnancy, and you may have a family history of depression and your own depression or anxiety risk factors. It should not be stigmatized. It makes women feel more isolated.
KB: How soon do you recommend that women who feel even an inkling of these feelings do something about it?
CH: Typically the "baby blues" will last a week or two, and that's a little bit of weepiness, mood swings and feeling overwhelmed. But once your body levels out, you move through that. When you hit week 3 or 4 and the feelings of distress are more intense or they're interfering with daily ability to function, then you definitely need to call your OB/GYN and tell them 'something's not right, can I come in and talk to you?' Don't wait until that six-week appointment.
KB: What are the options once they come in for help?
CH: We'll go over their symptoms, when they started and get a history. I always want to know how involved their OB office is and if their OB office is even aware this is happening and can help. Then find out if their symptoms are severe enough to warrant medication. Some OBs are willing to prescribe medications, but Austin also has female psychiatrists who specialize in postpartum issues with women and that's all they do. So we're very lucky that there are a lot of options in terms of therapy and medication and just getting support.
KB: Can women be treated without having to take medication?
CH: It's a case by case basis. Some women come in and the minute they know they have a place to go and talk, they start to feel better.
KB: How important is spousal/partner support?
CH: Very important. If the dads can be involved and I can educate the dads, it's so important. Women's success rate for pulling through postpartum distress is much higher if they have good support.
KB: How do you think we can better destigmatize postpartum issues?
CH: Education, education, education. Oftentimes I tell folks this is no different than if you have diabetes because it requires treatment, it requires you to be vigilant about the treatment, it requires you to make some changes and you can get through it.
KB: How long does it usually take?
CH: There are a lot of factors involved, like how much support they have from dads, support from family and the community. Are they able to access the care that's available?
Resources in Central Texas Help is available for mothers in the Austin-Round Rock area
The Pregnancy and Postpartum Health Alliance of Texas was created in May 2011 for moms in Central Texas. They offer three core programs for underserved mothers in the Austin community. These include a postpartum doula program, a therapy voucher program and a psychiatric voucher program. All of these are available to mothers who qualify and give care to those who might not be able to afford it otherwise.
Postpartum.net includes a "warm line," which is an 800 number women or their family members from all over the country can call and be connected with someone over the phone who can help in the moment.
The PostPartum Stress Center was founded by Karen Kleiman, who is well-known in the postpartum treatment field. She has written some very helpful books for new moms, trains practitioners and clinicians every year and works to bring awareness to PPD.
Seleni is an organization that works to train practitioners and provide information and resources for women.
NOTE: Some clinicians and practitioners will work on a sliding scale. Women need to ask if the practitioner is willing to do this.
PEOPLE ARE ALSO READING: